Cynthia Church, Chief Strategy Officer
This week, I’m in West Virginia visiting my mom – and the technology struggle is real. I am fortunate to be able to work remotely, although that isn’t an option when the internet is only somewhat reliable. This morning I woke to no broadband and a message that says:
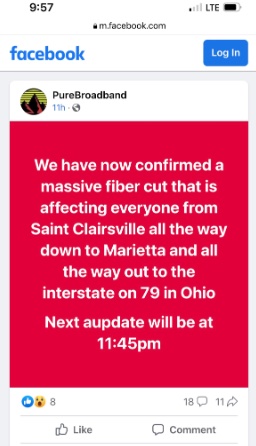 Now what? Good thing there is nothing mission-critical on the list for today. (Also, if anyone from Ohio or WV is reading this, stop trying to figure out where 79 goes through Ohio…it doesn’t. Clearly, they are frazzled.)
Now what? Good thing there is nothing mission-critical on the list for today. (Also, if anyone from Ohio or WV is reading this, stop trying to figure out where 79 goes through Ohio…it doesn’t. Clearly, they are frazzled.)
During the Reuters Digital Health Conference this spring, I attended a workshop where we were asked to think of barriers to accessing care, then specifically asked to exclude internet connectivity challenges because “there was nothing we could do about the infrastructure.”
Have we decided to accept that a lot of people lack affordable, reliable internet? Have we given up on trying to overcome this barrier?
We shouldn’t. Having grown up in the Mountain State, I know the people who live there, and in similar areas, and most do not fit the stereotypes. Many people choose to prioritize living within a community of extended family and friends over moving for economic gain.
We know this is harder, and we don’t always have access to the things that are readily available in a city, but mostly we’re willing to work a bit harder for them, with many people having to drive several hours to get to a mall or big box store.
Healthcare shouldn’t be something for which we have to work THAT much harder, just based on zip code. Digital health is often lauded as a way to reach those in rural communities, then in the next breath we write it off as too difficult due to lack of internet. I also often hear “rural” used as a substitute for low socio-economic. Yes, rural poverty is definitely an issue, but don’t forget there are many people in the country who do not fit that mold and are willing to meet you halfway to improve their access to care.
Healthcare systems who consider the needs of rural populations have a lot to gain – these people have to travel long distances for care regardless of where they go, so will chose from providers in a very wide radius from their home. When they have a good experience, they AND their caregivers will tell everyone else in their tight-knit community, “It’s a bit of a drive, but it’s worth it.”
Below are five relatively easy things we can do to make life easier for those without reliable internet, including me this week:
Mobile applications with offline functionality
Ask your mobile health vendors if their applications can function offline and synchronize data when an internet connection is available. This allows users to access and interact with health-related information even in areas with limited or no internet connectivity.
Offline health education materials
Develop offline educational materials, including pamphlets, posters, and video content, that are reasonable file sizes and can be downloaded when patients have access versus having to rely on a live website. Most rural folks are used to downloading and saving anything important because, well, internet.
Televisits – Plan B
Video visits are great until the internet drops suddenly, not to mention the anxiety of hoping for reliable internet connection in advance of the visit. There are security and privacy concerns, but don’t let them get in the way of patient care. If I have no internet connectivity, I can usually get enough cell reception to use WhatsApp video or FaceTime, even if Zoom or Teams isn’t an option, or use the landline to call someone (many people in areas with poor cell reception still have these old-fashioned devices with a cord attaching them to a wall and use them for “important” calls). Leveraging low-bandwidth technologies with optimized data transmission can help bridge the gap in healthcare access.
SMS, text messaging, and calling
Utilize SMS (Short Message Service) or text messaging services to deliver health-related information, reminders, and notifications to individuals who do not have reliable access to the internet. Also don’t forget the telephone – cell or landline – where you can send automated messages, as long as they are coming from the same telephone number with clear caller ID.
Avoid making assumptions
This is a human recommendation, not a technology one. When interacting with patients, ask about internet connectivity and IT literacy for them and their caregivers (remembering that people look after each other, so there are often multiple people involved in supporting a patient). Patients should be the ultimate decider on how they receive communication from their trusted care team; showing understanding of the challenges that patients face goes towards building that trust.
Maybe some of these ideas are basic, but from my vantage point at Xealth, I see these basic requirements de-prioritized. Are we expected to just wait until the government fixes the rural broadband issue?
If you have ideas of your own, or would like to brainstorm on all things digital health, please reach out!


